
Pertussis (Whooping Cough)
- January 15, 2026
- 1 Like
- 77 Views
- 0 Comments
Abstract
Pertussis (whooping cough) is a highly contagious bacterial respiratory infection notable for severe, prolonged coughing fits and for being especially dangerous in infants. This guide explains what pertussis is, typical symptoms across ages, how it spreads, why infants are at highest risk, how it is diagnosed and treated, and—most importantly—how it can be prevented (especially by vaccination and maternal immunization during pregnancy). The language is non-technical, globally relevant, and intended for patients, caregivers, and the general public. Key public-health actions (timely vaccination, seeking urgent care for young infants, and infection control at home) are emphasized. This guide is informational and not a substitute for direct medical advice.
Keywords: pertussis, whooping cough, infants, DTaP, Tdap, vaccination, azithromycin, prevention
Patient Education Guide (Main Text — APA style headings)
Introduction
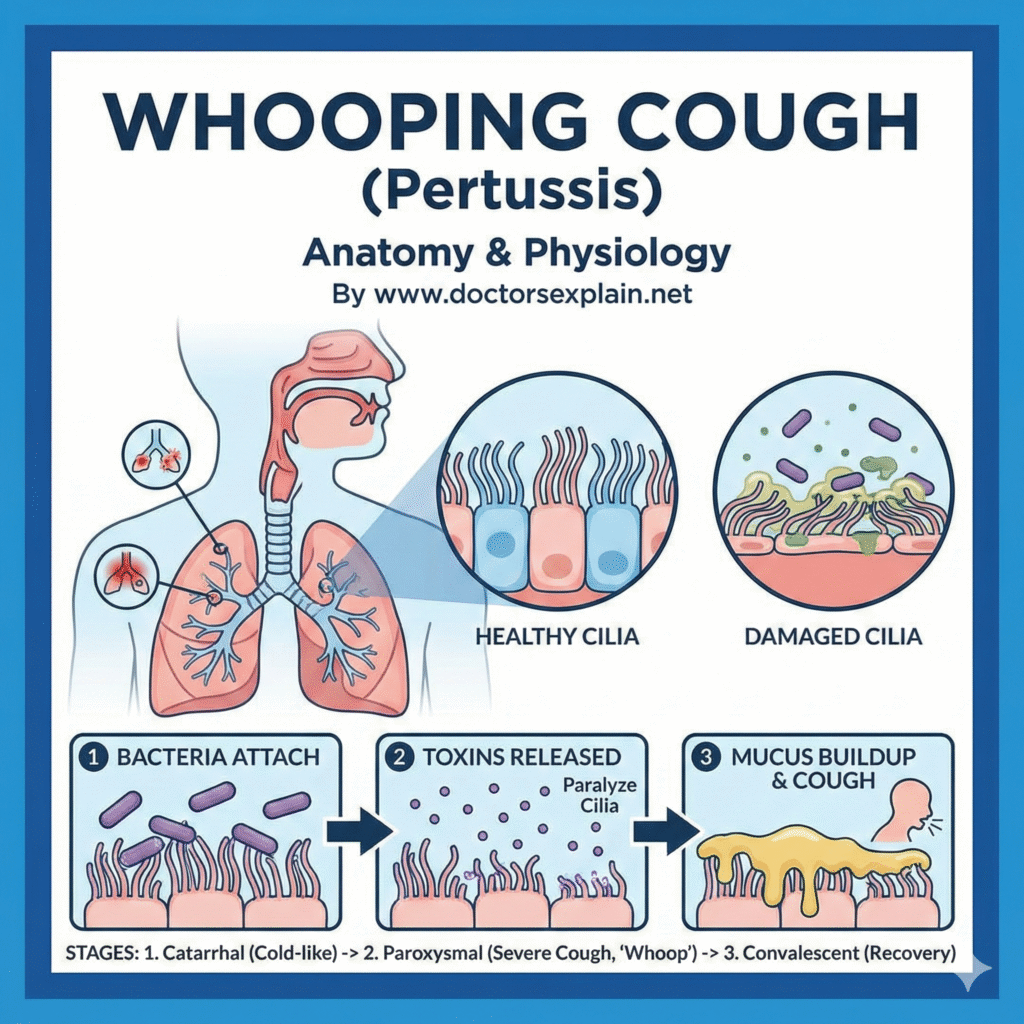
Pertussis, commonly called whooping cough, is caused by the bacterium Bordetella pertussis. It spreads easily through respiratory droplets when an infected person coughs or sneezes. While it can affect people of any age, it is most dangerous for babies too young to be fully vaccinated. Timely vaccination and early recognition of symptoms can prevent serious illness and death.
What is pertussis?
Pertussis is a bacterial respiratory infection that often begins like a mild cold—runny nose, low fever, and a mild cough—but may progress to repeated, violent coughing fits (paroxysms). In older children and adults the cough can be long-lasting; in infants it can cause life-threatening problems such as difficulty breathing, pauses in breathing (apnea), pneumonia, and even death.
Typical symptoms (by stage and age)
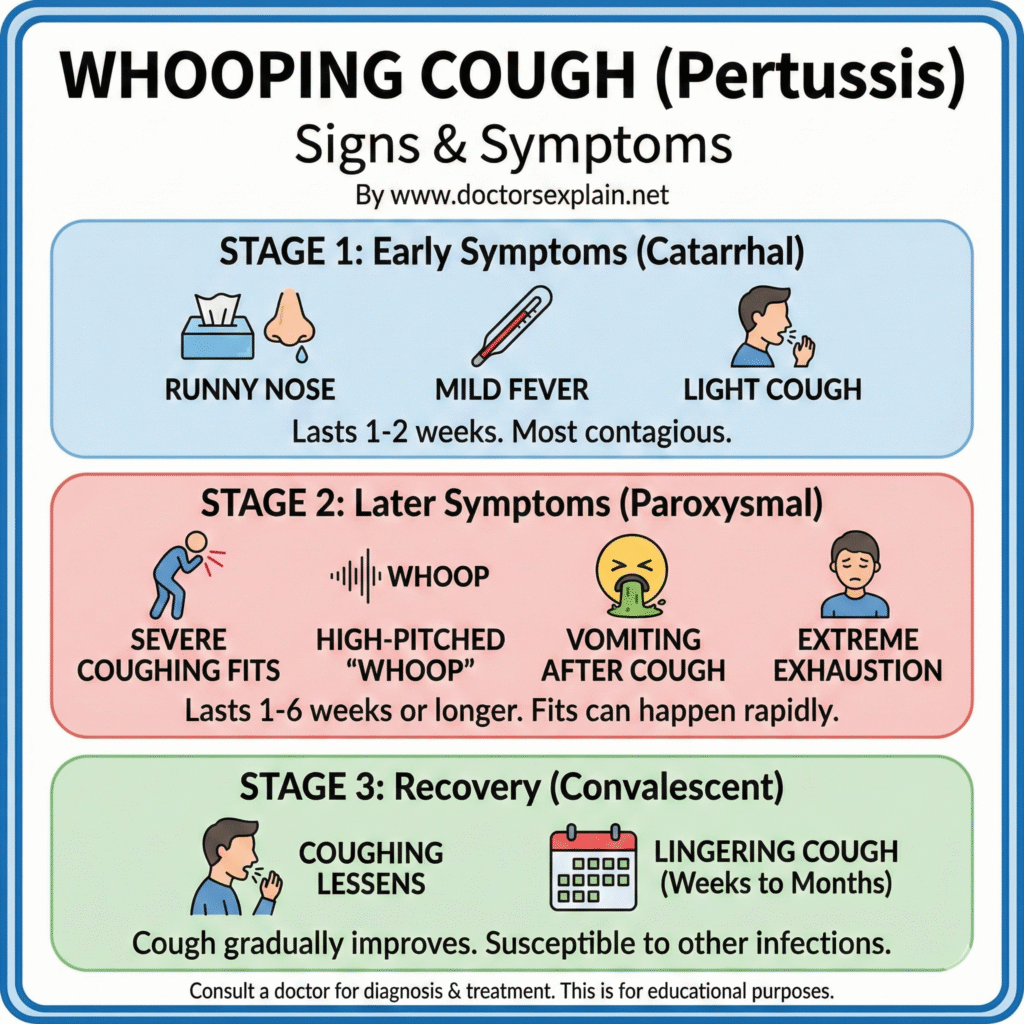
- Early (catarrhal) stage (1–2 weeks): mild cold-like symptoms — runny nose, sneezing, low fever, mild cough.
- Paroxysmal stage (weeks): severe coughing fits that may end with a high-pitched “whoop” (more common in young children), gagging, or vomiting after coughing. Older children and adults often have a prolonged cough without the classic whoop.
- Convalescent stage: cough gradually improves but may persist for many weeks (the “100-day cough” is a common phrase used to describe how long recovery can take).
Important note: Infants under 6 months may not make the whooping sound and instead may have very fast breathing, poor feeding, turning blue (cyanosis), or pauses in breathing. Any of these signs require immediate medical attention.
How pertussis spreads
Pertussis spreads when an infected person coughs or sneezes and another person breathes in the infected droplets, or has close contact with respiratory secretions. People are most contagious in the early stages, often before the severe cough begins, which makes control more difficult.
Who is at greatest risk?
- Young infants (especially <6 months): highest risk of severe disease, hospitalization, and death. Most infant cases are acquired from household contacts (often older siblings, parents, or caregivers).
- Pregnant people (if not immunized) and those with weakened immune systems also require special attention. Older children and adults are usually less severely ill but can transmit pertussis to infants.
Diagnosis
Diagnosis usually involves:
- A clinical history (pattern of cough and symptoms) and physical exam, and
- Laboratory testing in many cases: nasopharyngeal swab for PCR testing or culture; blood tests are less commonly used. Early testing helps guide treatment and public-health actions.
Treatment
- Antibiotics: Macrolide antibiotics (for example, azithromycin) are the usual first-line drugs for treatment and for preventing spread to close contacts; they are especially important for infants and pregnant contacts. Starting antibiotics early (ideally within the first 1–2 weeks) may reduce transmission to others; in older children and adults antibiotics may not shorten the coughing stage but are given to prevent spread. Azithromycin is commonly used for very young infants.
- Supportive care: For infants this may include hospitalization for breathing support, hydration, and monitoring. Adults and older children need rest, fluids, and monitoring for complications. Seek urgent care for babies with breathing problems, poor feeding, or lethargy.
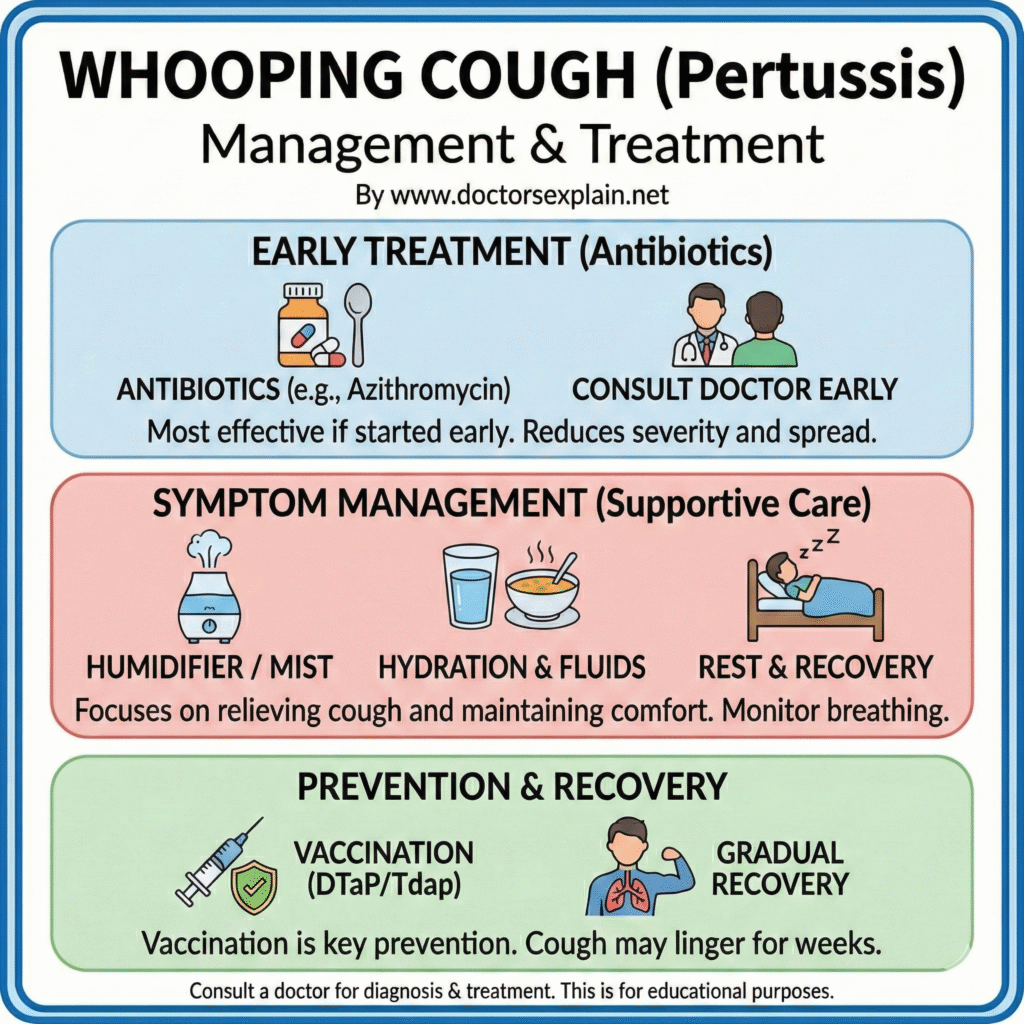
Prevention — Vaccination (the most important protection)
- Infant/child vaccine (DTaP): Most countries include pertussis-containing vaccines in early childhood schedules. The usual series begins at 2 months, 4 months, and 6 months of age, with additional booster doses in early childhood — follow your local national schedule. Timely infant vaccination greatly reduces the risk of severe disease.
- Adolescent/adult booster (Tdap): Older children, adolescents, and adults should receive Tdap booster doses as recommended by their national health authority to maintain immunity and reduce transmission.
- Maternal vaccination (Tdap during pregnancy): Receiving Tdap during each pregnancy—ideally between 27 and 36 weeks’ gestation—passes protective antibodies to the unborn baby and substantially reduces the baby’s risk of pertussis during the first months of life (before infant DTaP series is complete). This is strongly recommended in many countries.
Household “cocooning” and close-contact vaccination: Ensuring that caregivers, older siblings, and close contacts are up to date with Tdap helps protect infants who are too young to be fully vaccinated.
Infection control at home and in the community
- Isolate the sick person when possible, cover coughs/sneezes, practice hand hygiene, and avoid close contact with infants if you are coughing.
- If someone in the household has confirmed or suspected pertussis, public-health authorities may recommend antibiotics for close contacts and other measures to protect high-risk people (especially infants and pregnant people).
When to seek medical care (urgent signs)
Seek immediate medical care if:
- A baby or infant has coughing spells with difficulty breathing, turning blue, poor feeding, or pauses in breathing.
- Any person has severe, prolonged coughing that leads to vomiting, difficulty breathing, or fainting.
- You are pregnant and have been exposed to pertussis or have symptoms.
Frequently Asked Questions (FAQ)
Q: Can antibiotics cure the cough?
A: Antibiotics kill the bacteria and reduce spread, but they do not always shorten the duration of the coughing fits if started late. Early treatment reduces contagion.
Q: Is the “whoop” always present?
A: No. The classic “whoop” is more common in young children; infants may not whoop and instead may have apnea or difficulty breathing. Adults and older children may only have a long cough without the whoop.
Q: If I was vaccinated as a child, do I need more shots?
A: Immunity decreases over time. Tdap boosters for adolescents and adults, and especially Tdap during each pregnancy, are recommended by many health authorities. Check local guidance.
Practical advice for caregivers of infants
- Ensure pregnant people receive Tdap in pregnancy (27–36 weeks) to give newborn passive protection.
- Keep infant vaccination on schedule (DTaP at 2, 4, 6 months and follow-up boosters per national schedule).
- If an infant is exposed to pertussis, contact a healthcare provider immediately—antibiotic prophylaxis and close monitoring may be advised.
Limitations and final note
This guide is intended for general public education. Individual medical decisions depend on personal health history, local disease patterns, and national immunization schedules. Always consult a healthcare professional or local public-health authority for diagnosis, treatment, and local vaccination guidance.
References
Centers for Disease Control and Prevention. (n.d.). Pertussis (whooping cough). CDC.
Centers for Disease Control and Prevention. (n.d.). Whooping cough (pertussis) — Vaccination recommendations. CDC.
Centers for Disease Control and Prevention. (n.d.). Tdap vaccination during pregnancy. CDC.
World Health Organization. (2024). Pertussis: What you need to know (factsheet). WHO.
National Health Service (NHS). (n.d.). Whooping cough — NHS. NHS.
American College of Obstetricians and Gynecologists (ACOG). (2017). Update on immunization and pregnancy: Tdap vaccination (Committee Opinion).
Public Health England / UK Health Security Agency (news). (2024). Reporting and situational updates on infant deaths and outbreaks (example news reporting of infant risk).



Leave Your Comment